Antibiotics
In common usage, an antibiotic (from the Ancient Greek: ἀντί – anti, "against", and βίος – bios, "life") is a substance or compound that kills or inhibits the growth of bacteria. Antibiotics belong to the broader group of antimicrobial compounds, used to treat infections caused by microorganisms, including fungi and protozoa.
The term "antibiotic" was coined by Selman Waksman in 1942 to describe any substance produced by a microorganism that is antagonistic to the growth of other microorganisms in high dilution. This original definition excluded naturally occurring substances that kill bacteria but are not produced by microorganisms (such as gastric juice and hydrogen peroxide) and also excluded synthetic antibacterial compounds such as the sulfonamides. Many antibiotics are relatively small molecules with a molecular weight less than 2000 Da.
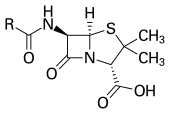
With advances in medicinal chemistry, most antibiotics are now semisynthetic — modified chemically from original compounds found in nature, as is the case with beta-lactams (which include the penicillins, produced by fungi in the genus Penicillium, the cephalosporins, and the carbapenems). Some antibiotics are still produced and isolated from living organisms, such as the aminoglycosides, and others have been created through purely synthetic means: the sulfonamides, the quinolones, and the oxazolidinones. In addition to this origin-based classification into natural, semisynthetic, and synthetic, antibiotics may be divided into two broad groups according to their effect on microorganisms: those that kill bacteria are bactericidal agents, while those that only impair bacterial growth are known as bacteriostatic agents.
Antibiotic resistance
The emergence of antibiotic resistance is an evolutionary process that is based on selection for organisms that have enhanced ability to survive doses of antibiotics that would have previously been lethal. Antibiotics like Penicillin and Erythromycin which used to be one-time miracle cures are now less effective because bacteria have become more resistant. Antibiotics themselves act as a selective pressure which allows the growth of resistant bacteria within a population and inhibits susceptible bacteria. Antibiotic selection of pre-existing antibiotic resistant mutants within bacterial populations was demonstrated in 1943 by the Luria-Delbrück experiment. Survival of bacteria often results from an inheritable resistance. Any antibiotic resistance may impose a biological cost and the spread of antibiotic resistant bacteria may be hampered by the reduced fitness associated with the resistance which proves disadvantageous for survival of the bacteria when antibiotic is not present. Additional mutations, however, may compensate for this fitness cost and aids the survival of these bacteria.
The underlying molecular mechanisms leading to antibiotic resistance can vary. Intrinsic resistance may naturally occur as a result of the bacteria's genetic makeup. The bacterial chromosome may fail to encode a protein which the antibiotic targets. Acquired resistance results from a mutation in the bacterial chromosome or the acquisition of extra-chromosomal DNA. Antibiotic-producing bacteria have evolved resistance mechanisms which have been shown to be similar to and may have been transferred to antibiotic resistant strains. The spread of antibiotic resistance mechanisms occurs through vertical transmission of inherited mutations from previous generations and genetic recombination of DNA by horizontal genetic exchange. Antibiotic resistance exchanged between different bacteria by plasmids that carry genes which encode antibiotic resistance which may result in co-resistance to multiple antibiotics. These plasmids can carry different genes with diverse resistance mechanisms to unrelated antibiotics but because they are located on the same plasmid multiple antibiotic resistance to more than one antibiotic is transferred. Alternatively, cross-resistance to other antibiotics within the bacteria results when the same resistance mechanism is responsible for resistance to more than one antibiotic is selected for.
| Generic name | Brand names | Common uses | Possible side effects | Mechanism of action | |
|---|---|---|---|---|---|
| Aminoglycosides | |||||
| Amikacin | Amikin | Infections caused by Gram-negative bacteria, such as Escherichia coli and Klebsiella particularly Pseudomonas aeruginosa. Effective against Aerobic bacteria (not obligate/facultative anaerobes) and tularemia. |
|
Binding to the bacterial ribosomal subunit (some work by binding to the 50S subunit), inhibiting the translocation of the peptidyl-tRNA from the A-site to the P-site and also causing misreading of mRNA, leaving the bacterium unable to synthesize proteins vital to its growth. | |
| Gentamicin | Garamycin | ||||
| Kanamycin | Kantrex | ||||
| Neomycin | Mycifradin | ||||
| Netilmicin | Netromycin | ||||
| Streptomycin | |||||
| Tobramycin | Nebcin | ||||
| Paromomycin | Humatin | ||||
| Ansamycins | |||||
| Geldanamycin | Experimental, as antitumor antibiotics | ||||
| Herbimycin | |||||
| Carbacephem | |||||
| Loracarbef | Lorabid | prevents bacterial cell division by inhibiting cell wall synthesis. | |||
| Carbapenems | |||||
| Ertapenem | Invanz | Bactericidal for both Gram-positive and Gram-negative organisms and therefore useful for empiric broad-spectrum antibacterial coverage. (Note MRSA resistance to this class.) |
|
Inhibition of cell wall synthesis | |
| Doripenem | Finibax | ||||
| Imipenem/Cilastatin | Primaxin | ||||
| Meropenem | Merrem | ||||
| Cephalosporins (First generation) | |||||
| Cefadroxil | Duricef |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. | ||
| Cefazolin | Ancef | ||||
| Cefalotin or Cefalothin | Keflin | ||||
| Cefalexin | Keflex | ||||
| Cephalosporins (Second generation) | |||||
| Cefaclor | Ceclor |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. | ||
| Cefamandole | Mandole | ||||
| Cefoxitin | Mefoxin | ||||
| Cefprozil | Cefzil | ||||
| Cefuroxime | Ceftin, Zinnat | ||||
| Cephalosporins (Third generation) | |||||
| Cefixime | Suprax |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. | ||
| Cefdinir | Omnicef, Cefdiel | ||||
| Cefditoren | Spectracef | ||||
| Cefoperazone | Cefobid | ||||
| Cefotaxime | Claforan | ||||
| Cefpodoxime | Vantin | ||||
| Ceftazidime | Fortaz | ||||
| Ceftibuten | Cedax | ||||
| Ceftizoxime | |||||
| Ceftriaxone | Rocephin | ||||
| Cephalosporins (Fourth generation) | |||||
| Cefepime | Maxipime |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. | ||
| Cephalosporins (Fifth generation) | |||||
| Ceftobiprole | Used to treat MRSA |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. | ||
| Glycopeptides | |||||
| Teicoplanin | inhibiting peptidoglycan synthesis | ||||
| Vancomycin | Vancocin | ||||
| Macrolides | |||||
| Azithromycin | Zithromax, Sumamed, Zitrocin | Streptococcal infections, syphilis, respiratory infections, mycoplasmal infections, Lyme disease |
|
inhibition of bacterial protein biosynthesis by binding irreversibly to the subunit 50S of the bacterial ribosome, thereby inhibiting translocation of peptidyl tRNA. | |
| Clarithromycin | Biaxin | ||||
| Dirithromycin | Dynabac | ||||
| Erythromycin | Erythocin, Erythroped | ||||
| Roxithromycin | |||||
| Troleandomycin | TAO | ||||
| Telithromycin | Ketek | Pneumonia | Visual Disturbance, Liver Toxicity. | ||
| Spectinomycin | Antimetabolite, Anticancer | ||||
| Monobactams | |||||
| Aztreonam | Azactam | Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. | |||
| Penicillins | |||||
| Amoxicillin | Novamox, Amoxil | Wide range of infections; penicillin used for streptococcal infections, syphilis, and Lyme disease |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. | |
| Ampicillin | Principen | ||||
| Azlocillin | |||||
| Carbenicillin | |||||
| Cloxacillin | Tegopen | ||||
| Dicloxacillin | Dynapen | ||||
| Flucloxacillin | Floxapen | ||||
| Mezlocillin | |||||
| Meticillin | |||||
| Nafcillin | |||||
| Oxacillin | |||||
| Penicillin | |||||
| Piperacillin | |||||
| Ticarcillin | |||||
| Polypeptides | |||||
| Bacitracin | Eye, ear or bladder infections; usually applied directly to the eye or inhaled into the lungs; rarely given by injection | Kidney and nerve damage (when given by injection) | Inhibits isoprenyl pyrophosphate, a molecule which carries the building blocks of the peptidoglycan bacterial cell wall outside of the inner membrane | ||
| Colistin | Interact with the bacterial cytoplasmic membrane, changing its permeability. | ||||
| Polymyxin B | |||||
| Quinolones | |||||
| Ciprofloxacin | Cipro, Ciproxin, Ciprobay | Urinary tract infections, bacterial prostatitis, community-acquired pneumonia, bacterial diarrhea, mycoplasmal infections, gonorrhea | Nausea (rare), irreversible damage to central nervous system (uncommon), tendinosis (rare) | inhibit the bacterial DNA gyrase or the topoisomerase IV enzyme, thereby inhibiting DNA replication and transcription. | |
| Enoxacin | Penetrex | ||||
| Gatifloxacin | Tequin | ||||
| Levofloxacin | Levaquin | ||||
| Lomefloxacin | Maxaquin | ||||
| Moxifloxacin | Avelox | ||||
| Norfloxacin | Noroxin | ||||
| Ofloxacin | Floxin, Ocuflox | ||||
| Trovafloxacin | Trovan | Withdrawn | |||
| Grepafloxacin | Raxar | Withdrawn | |||
| Sparfloxacin | Zagam | Withdrawn | |||
| Temafloxacin | Omniflox | Withdrawn | |||
| Sulfonamides | |||||
| Mafenide | Urinary tract infections (except sulfacetamide and mafenide); mafenide is used topically for burns |
|
Folate synthesis inhibition. They are competitive inhibitors of the enzyme dihydropteroate synthetase, DHPS. DHPS catalyses the conversion of PABA (para-aminobenzoate) to dihydropteroate, a key step in folate synthesis. Folate is necessary for the cell to synthesize nucleic acids (nucleic acids are essential building blocks of DNA and RNA), and in its absence cells will be unable to divide. | ||
| Sulfonamidochrysoidine (archaic) | Prontosil | ||||
| Sulfacetamide | |||||
| Sulfadiazine | Micro-Sulfon | ||||
| Sulfamethizole | |||||
| Sulfanilimide (archaic) | |||||
| Sulfasalazine | Azulfidine | ||||
| Sulfisoxazole | |||||
| Trimethoprim | Trimpex | ||||
| Trimethoprim-Sulfamethoxazole (Co-trimoxazole) (TMP-SMX) | Bactrim, Septra | ||||
| Tetracyclines | |||||
| Demeclocycline | Declomycin | Syphilis, chlamydial infections, Lyme disease, mycoplasmal infections, acne rickettsial infections, malaria. Note: Malaria is caused by a protist and not a bacterium. |
|
inhibiting the binding of aminoacyl-tRNA to the mRNA-ribosome complex. They do so mainly by binding to the 30S ribosomal subunit in the mRNA translation complex. | |
| Doxycycline | Vibramycin | ||||
| Minocycline | Minocin | ||||
| Oxytetracycline | Terramycin | ||||
| Tetracycline | Sumycin, Achromycin V, Steclin | ||||
| Others | |||||
| Arsphenamine | Salvarsan | Spirochaetal infections (obsolete) | |||
| Chloramphenicol | Chloromycetin | meningitis, | Rarely: aplastic anemia. |
Inhibits bacterial protein synthesis by binding to the 50S subunit of the ribosome |
| |
| Clindamycin | Cleocin | acne infections, prophylaxis before surgery | |||
| Lincomycin | Lincocin | acne infections, prophylaxis before surgery | |||
| Ethambutol | Myambutol | Antituberculosis | |||
| Fosfomycin | Monurol | ||||
| Fusidic acid | Fucidin | ||||
| Furazolidone | |||||
| Isoniazid | I.N.H. | Antituberculosis | |||
| Linezolid | Zyvox | VRSA | |||
| Metronidazole | Flagyl | Giardia | |||
| Mupirocin | Bactroban | ||||
| Nitrofurantoin | Macrodantin, Macrobid | ||||
| Platensimycin | |||||
| Pyrazinamide | Antituberculosis | ||||
| Quinupristin/Dalfopristin | Syncercid | ||||
| Rifampicin (Rifampin in US) | mostly Gram-positive and mycobacteria | Reddish-orange sweat, tears, and urine | Binds to the β subunit of RNA polymerase to inhibit transcription | ||
| Thiamphenicol | Gram-negative, Gram-positive, anaerobes. Widely used in veterinary medicine. | Lacks known anemic side-effects. | A chloramphenicol analog. May inhibit bacterial protein synthesis by binding to the 50S subunit of the ribosome | ||
| Tinidazole | |||||
| Dapsone | Avlosulfon | Antileprotic | |||
| Lamprene |
Antileprotic |
|
|
| |
| Generic Name | Brand Names | Common Uses | Possible Side Effects | Mechanism of action | |









